

The most commonly cited is the Robert David Cerfolio Classification System ( 6). A few classifications have attempted to quantify air leaks. Grading of the air leak is done by recording the numbered column the bubbles reach when the patient coughs or exhales the higher the number reached the larger the air leak.

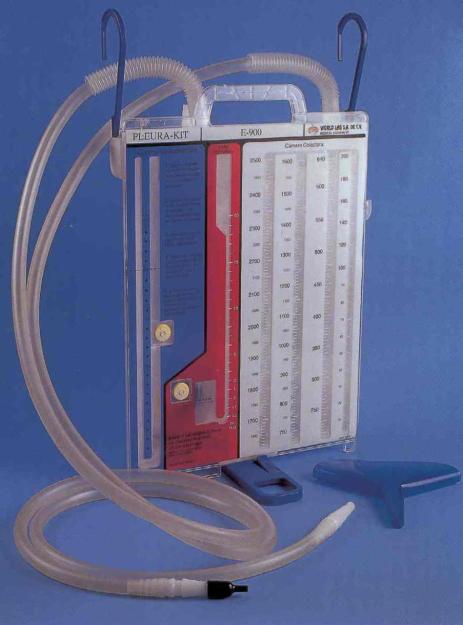
An air leak is measured by bubbling in the water seal chamber. These devices consist of a collection chamber for fluid and a water seal chamber for measurement of air leak. The most common devices used today are the Pleur-evac (Teleflex Incorporated, USA) and Atrium (Maquet Getinge Group, Germany) systems. The dry suction system allows for higher suction pressures. Current analogue drainage systems comprise of wet or dry suction controls. Initial chest drainage devices were based on a three-bottle system. It is important to note the assessment discussed below is limited to an air leak from alveolar-pleural fistula and not a broncho-pleural fistula (BPF), which requires a more complex assessment and management plan.
Pleur evac atrium portable#
And, patients are being discharged with portable devices and therefore requiring outpatient assessment of air leaks.

The role of routine chest X-rays (CXR) has also been recently reconsidered. Digital devices have allowed more objective measurements of air leaks by measuring and recording the continuous airflow as volume per time (i.e., mL/min).
Traditional analogue devices only allow for a subjective static assessment of air leaks. The accurate measurement of an air leak following lung resection has come to the forefront of ERAS programs. This manuscript will focus on the two components of postoperative management of PAL: (I) accurate assessment of the air leak, and (II) management of a true alveolar-pleural fistula. Management of air leaks spans from the preoperative assessment to predict patients at high risk of PAL, intraoperative maneuvers to prevent parenchymal air leaks and postoperative management to reduce the duration of an air leak. Over 50% of patients undergoing lung resection will have an air leak within the first 24 hours after surgery ( 2- 4) and up to 15% of patients will have a PAL ( 5).Įnhanced recovery after surgery (ERAS) programs must be designed to deal with air leaks in a systemic, evidence-based manner. Despite multiple advances in lung resection, including the use of stapling devices, sealants and approaches without fissure dissection, thoracic surgeons continue to be plagued by air leaks. Prolonged air leaks (PAL) have been defined as lasting more than 5 days after surgery ( 2). They result from an alveolar-pleural fistula, and in most instances, will heal spontaneously. Post-lung resection air leaks remain one of the most common complications resulting in delay of hospital discharge ( 1). Keywords: Enhanced recovery after surgery (ERAS) chest drain protocol chest tube management Standardization of postoperative care through ERAS programs will allow for the design of larger RCTs to better understand some of the controversies around the management of postoperative air leaks. There is also literature to support the design of protocols for management of postoperative air leaks.
Pleur evac atrium Patch#
The key findings are that a single chest drain is adequate in the majority of cases to manage an air leak, the use of applied external suction is unlikely to prevent or prolong an air leak, autologous blood patch pleurodesis may potentially shorten postoperative air leaks and there is sufficient data to support that patients can safely be discharged with a portable drainage system. The literature regarding the management of postoperative air leaks, including the number of chest tubes, the role of applied external suction, invasive maneuvers and discharge with a portable device is reviewed. Published data suggests that digital drainage systems result in a more confident assessment of air leaks. Accurate assessment of air leaks using traditional analogues devices, newer digital drainage systems, portable devices and chest X-rays (CXR) are reviewed. ERAS programs should consider two components when creating protocols for air leaks: assessment and management. Enhanced recovery after surgery (ERAS) programs must be designed to manage parenchymal air leaks. Abstract: Air leaks are the most common complication after pulmonary resection.


 0 kommentar(er)
0 kommentar(er)
